
So far in this series (view Part One here; Part Two here), we've given an overview of vital signs. In this next segment, we'll go into what they represent in terms of patient physiology and clinical significance. Watch the video below or keep reading to dive in.
Vital signs allow the EMT to observe a patient's condition and determine if it's stable, improving, or worsening. By collecting vitals at regular intervals, the EMT is able to observe trends in the patient's condition and prepare resources and response appropriately. Elevations in pulse and respiratory rate indicate activation of the patient's sympathetic nervous system, the branch of the autonomic nervous system responsible for governing the adrenal or fight-or-flight response.
A patient exhibiting elevated pulse or respiratory rate is working hard to keep tissues perfused and may be suffering from hypovolemia, respiratory distress, or a ventilation-perfusion mismatch. A state of inadequate perfusion is called shock and is a result of the body changing ventilation, pulse, and 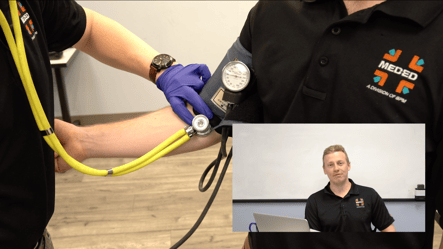 blood flow throughout the body in order to keep vital organs perfused. In addition to elevations in heart and respiratory rate, shock also presents with pale, cool, clammy, or diaphoretic skin and altered mental status. In the condition of shock, blood pressure may stay the same or increase early on and gradually decline as the patient's compensatory mechanisms begin to tire and fail as the patient enters decompensated shock. Be on the lookout for an upcoming video on the pathophysiology of shock.
blood flow throughout the body in order to keep vital organs perfused. In addition to elevations in heart and respiratory rate, shock also presents with pale, cool, clammy, or diaphoretic skin and altered mental status. In the condition of shock, blood pressure may stay the same or increase early on and gradually decline as the patient's compensatory mechanisms begin to tire and fail as the patient enters decompensated shock. Be on the lookout for an upcoming video on the pathophysiology of shock.
When interpreting blood pressure in all patients, remember that hypotension means inadequate pressure to perfused tissues; and hypertension can increase likelihood of stroke, heart attack, or aneurysm. A patient's medical history and current medications are also important to consider.
Pulse oximetry is a useful but sometimes limited tool for determining a patient's blood oxygenation status. When interpreting a pulse oximetry reading, remember to consider other clinical findings and intervene if the patient shows signs of hypoxia such as cyanosis, anxiety, altered mental status, tripod positioning, or respiratory distress.
 Low blood sugar or hypoglycemia can cause severely depressed mental status, loss of consciousness, seizures, or depression in respiratory rate. Hypoglycemia is a severe medical emergency that must be intervened upon quickly depending on your scope and local protocols. A state of high blood sugar or hyperglycemia is also a serious medical condition but sometimes presents with slower onset. There are few interventions, besides rapid transport, available to basic level EMS providers.
Low blood sugar or hypoglycemia can cause severely depressed mental status, loss of consciousness, seizures, or depression in respiratory rate. Hypoglycemia is a severe medical emergency that must be intervened upon quickly depending on your scope and local protocols. A state of high blood sugar or hyperglycemia is also a serious medical condition but sometimes presents with slower onset. There are few interventions, besides rapid transport, available to basic level EMS providers.
After initially determining your patient's level of responsiveness with AVPU or GCS, continually reassess by talking to your patient and building a rapport, constantly observing for changes in responsiveness. A once talkative patient who becomes increasingly calm or quiet may not be improving, rather they may be experiencing a decline in mental status.
This wraps up our general overview of vital signs for pre-hospital EMS providers. Follow Best Practice Medicine (on our BPM TV YouTube Channel!) to stay informed on all things medical so when the emergency hits, you're ready.
Want to learn more? Sign up for one of our upcoming EMT courses today or check out one of our many other course offerings!

