
This is the second installation of our 3-part overview of vital signs in pre-hospital settings. In this portion we will be talking about pulse oximetry, blood glucometry and the mental assessment scale AVPU. To review the content in the first installment on vitals check out our previous blog post: Learning and Obtaining Vitals Pt. 1 of 3. Watch our video below or keep reading for more.
Pulse oximetry is a somewhat limited vital sign, in that its accuracy depends on the conditions in which the measurement is taken. A cold environment reduces the amount of blood flowing through the peripheral tissues and can affect the accuracy of the measurement. And nail polish interferes with the beam of light emitted by the device.
Patients with carbon monoxide poisoning will show a falsely high pulse oximetry reading due to similarity between the way carbon monoxide binds with hemoglobin and the way oxygen binds with hemoglobin.
Additionally, SPO2 measured on patients in a severe hypovolemic state may show adequate oxygenation of greater than 96%, despite the fact the patient being in sever shock, simply due to the lack of enough oxygenated blood to circulate through the tissues (i.e. internal hemorrhage).

Blood glucometry gives the provider a reading of how much glucose is dissolved and circulating through the body's tissues. Glucose is the fuel all the body's cells use to make energy and without an adequate level of glucose available to the tissues, organs will fail to function properly. A blood glucometry kit consists of a glucometer, alcohol prep swabs, lancets to pierce the patient’s skin, and test strips to sample the blood.
 Prep the injection site using an alcohol swab. Most patients appreciate using a site on the side of their finger, so you don't leave a pinpoint on the pad that they'll feel when they use their hand later. Prepare the glucometer by inserting a test strip, making sure that the collection channel is out and visible. Most modern glucometers will automatically turn on upon the insertion of a test strip. Once the sampling site is dry, use a lancet to make a small pinprick and squeeze a droplet of the patients blood. Make sure you have a big enough droplet to completely fill the channel of the collection device. Gently touch the collection channel with a droplet, allowing blood to run all the way up to the top, at which time, the glucometer will automatically generate a reading.
Prep the injection site using an alcohol swab. Most patients appreciate using a site on the side of their finger, so you don't leave a pinpoint on the pad that they'll feel when they use their hand later. Prepare the glucometer by inserting a test strip, making sure that the collection channel is out and visible. Most modern glucometers will automatically turn on upon the insertion of a test strip. Once the sampling site is dry, use a lancet to make a small pinprick and squeeze a droplet of the patients blood. Make sure you have a big enough droplet to completely fill the channel of the collection device. Gently touch the collection channel with a droplet, allowing blood to run all the way up to the top, at which time, the glucometer will automatically generate a reading.
Several different scales are used to determine a patients mental status. The first and simplest is called the AVPU scale. AVPU stands for alert, verbal, painful and unresponsive. If a patient is conscious and alert, their alertness is classified based on how oriented they are to their person, place, time and events. If your patient is fully oriented to person, place, time and events, they're reported as being A&O four out of four.
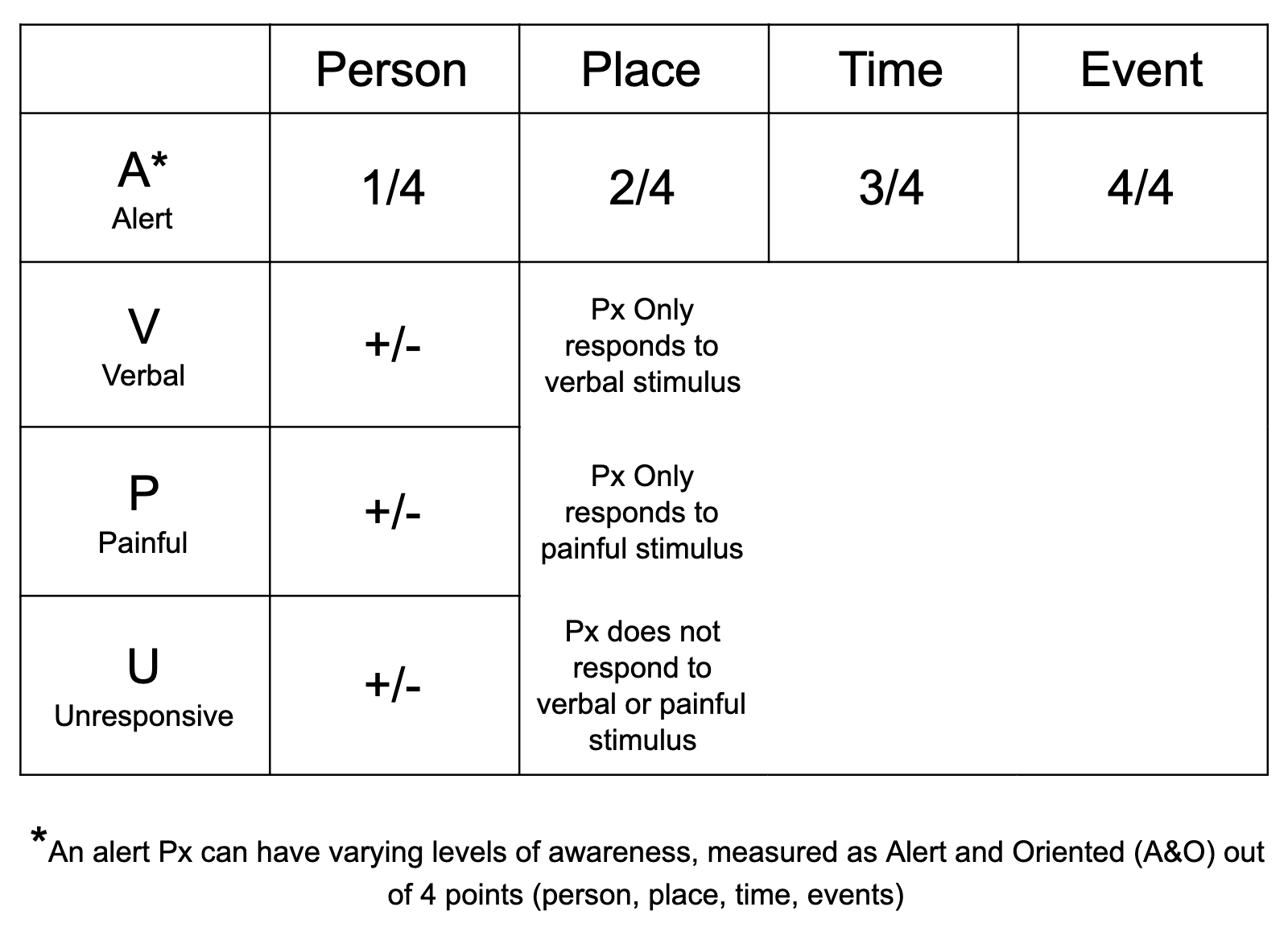
A patient who's only able to answer three of the questions is reported as being A&O three out of four. If a patient is less than alert and awake, they're given progressively a verbal stimulus or a painful stimulus to determine their responsiveness level. A person who does not respond to verbal or painful stimulus is unresponsive.
A patients blood oxygen saturation should be around 96% in a healthy adult. While normal blood oxygen saturation levels may vary, any patient exhibiting signs of hypoxia with a pulse oximetry reading of less than 92-94% should be given supplemental oxygen.
Blood glucose is measured in milligrams per deciliter. A normal range for a healthy adult is in between 60-120. And unlike the other two vital signs discussed above, the AVPU scale is a qualitative, rather than quantitative measurement.
Any healthy adult should receive a normal four out of four points on the alert and oriented scale. Anything less than this is an indication of altered mental status.
Depending on scope and capacity within an EMS system, different practitioners may include other metrics as vital signs, such as exact body temperature, pulse pressure, and body mass index. For simplification we will not be reviewing these additional vitals as they have less prevalence in pre-hospital EMS settings.
Join us again for our final installation on vital signs reviewing the measurements we use as EMTs to assess the trend of patients. Follow Best Practice Medicine (on our BPM TV YouTube Channel) to stay informed on all things medical so when the emergency hits, you're ready.
Want to learn more? Sign up for one of our upcoming EMT courses today or check out one of our many other course offerings!

